November 2021
What Can I Do When a Wound Doesn’t Heal?
If you have a wound for more than 8 weeks and it still hasn’t healed, it may be considered to be chronic. Such an occurrence could be caused by poor circulation, diabetes, or a weak immune system. Open wounds on the lower leg are known as venous leg ulcers. These kinds of wounds may be medically treated by removing the dead or inflamed tissue, known as debridement. The wound itself can then be cleaned by a high-pressure water jet. A local anesthetic may be used as this treatment is said to be painful. Afterward, the wound should be covered with gauze or a similar dressing to keep it from becoming infected. Compression stockings may be prescribed to increase circulation. For more information on chronic wounds in the feet or ankle area, please consult a podiatrist.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with John McGhan, DPM from Gold Canyon Foot & Ankle. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our office located in Gold Canyon, AZ . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Wound Care
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.
Stretches to Help Improve Plantar Fasciitis
When the fibrous tissue on the sole that connects the heel with the front of the foot (plantar fascia) becomes damaged and inflamed, this is known as plantar fasciitis. Plantar fasciitis can also cause tense muscles in other parts of the foot and calf. Sometimes stretches can ease some of this tension and discomfort in these muscles as well as the plantar fascia. Simple calf stretches are a good place to start. To get a good stretch in the affected foot, place it behind you—flat on the ground—with the leg and knee straight. The other leg should be bent in front of you with that foot also lying flat, and your hands placed against a wall in front of you. Hold that position for 10 seconds and then release. You should feel an easy stretch in the calf and heel of the affected foot. Rolling a foam roller or ball back and forth under the affected foot while seated can also provide a good stretch in the foot. For another gentle calf stretch, sit on a chair and either curl a towel on the floor or pick up marbles with your toes. If your plantar fasciitis does not improve or is severe, a podiatrist can offer many solutions to treat it.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact John McGhan, DPM from Gold Canyon Foot & Ankle. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
- Excessive running
- Non-supportive shoes
- Overpronation
- Repeated stretching and tearing of the plantar fascia
How Can It Be Treated?
- Conservative measures – anti-inflammatories, ice packs, stretching exercises, physical therapy, orthotic devices
- Shockwave therapy – sound waves are sent to the affected area to facilitate healing and are usually used for chronic cases of plantar fasciitis
- Surgery – usually only used as a last resort when all else fails. The plantar fascia can be surgically detached from the heel
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your doctor right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions please feel free to contact our office located in Gold Canyon, AZ . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Plantar Fasciitis
The plantar fascia is a connective tissue in the heel that stretches across the bottom length of your foot. Plantar fasciitis occurs when the connective tissue becomes inflamed, causing heel pain and discomfort during physical activity. Although the condition is completely treatable, traditional methods can take up to a year to start becoming effective.
Plantar fasciitis is caused by a number of everyday activities, so understanding the condition is important for managing and treating it. One of the most common causes of plantar fasciitis is excessive running, especially with improper fitting or non-supportive shoes. Too much exercise can lead to the plantar fascia being overworked and overstretched, which can cause tears in the tissue. Along with improper fitting shoes, pronation, the rolling of the feet inward, is a common cause of plantar fasciitis. If not treated properly, the plantar fascia becomes overstretched and starts to tear, causing inflammation.
Despite the common causes of plantar fasciitis, there are many different treatment options. For less severe cases, conservative home remedies include taking anti-inflammatory drugs to alleviate pain, applying ice packs to the bottom of your foot and heel, slowly stretching and exercising your feet to re-strengthen the tissue, and using orthotic devices are all ways to help manage your plantar fasciitis.
For more severe cases, shockwave therapy has become a common solution for plantar fasciitis. Shockwave therapy can effectively break up the tissue on the bottom of your foot which facilitates healing and regeneration. This fights the chronic pain caused by plantar fasciitis. Even if this doesn’t work, surgery is always a final option. Surgery on the tissue itself can be done to permanently correct the issue and stop the inflammation and pain in your heels.
No matter what the case may be, consulting your podiatrist is the first and best step to recovery. Even the slightest amount of heel pain could be the first stage of plantar fasciitis. Untreated symptoms can lead to the tearing and overstretching of tissue. Because the tearing of tissue can be compounded if it remains ignored, it can evolve into a severe case. The solution is early detection and early treatment. Talk to your podiatrist about the possibilities of plantar fasciitis if you’re experiencing heel pain.
Why Heel Spurs Form
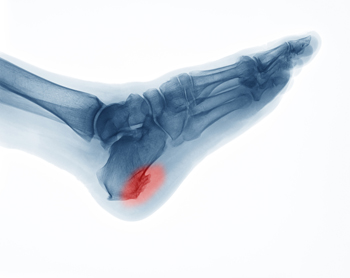
Heel Spurs are calcium deposits that form on the bottom of the heel near the arch. This area of the foot is referred to as the plantar fascia. Heel spurs can occur when the heel bone and plantar fascia are exposed to repeated stress. This type of stress can be due to over-stretching the plantar fascia, habitual tearing of the heel bone’s thin lining, and straining ligaments and muscles in the feet. The stress in this area usually also causes plantar fasciitis (an inflammation of the plantar fascia). Because heel spurs are not always painful, and usually occur along with plantar fasciitis, they can often go undetected. Symptomatic heel spurs can create a sharp pain, inflammation and tenderness, and feel warm to the touch. People who are obese, older, or who wear improper footwear, are more at risk of developing heel spurs, as well as those who participate in activities such as running and jumping repeatedly, or who suffer from osteoarthritis. A podiatrist will typically use X-rays to identify and diagnose heel spurs. If you believe you may have heel spurs, make an appointment with a podiatrist for an examination and analysis of your condition.
Heel spurs can be incredibly painful and sometimes may make you unable to participate in physical activities. To get medical care for your heel spurs, contact John McGhan, DPM from Gold Canyon Foot & Ankle. Our doctor will do everything possible to treat your condition.
Heels Spurs
Heel spurs are formed by calcium deposits on the back of the foot where the heel is. This can also be caused by small fragments of bone breaking off one section of the foot, attaching onto the back of the foot. Heel spurs can also be bone growth on the back of the foot and may grow in the direction of the arch of the foot.
Older individuals usually suffer from heel spurs and pain sometimes intensifies with age. One of the main condition's spurs are related to is plantar fasciitis.
Pain
The pain associated with spurs is often because of weight placed on the feet. When someone is walking, their entire weight is concentrated on the feet. Bone spurs then have the tendency to affect other bones and tissues around the foot. As the pain continues, the feet will become tender and sensitive over time.
Treatments
There are many ways to treat heel spurs. If one is suffering from heel spurs in conjunction with pain, there are several methods for healing. Medication, surgery, and herbal care are some options.
If you have any questions feel free to contact our office located in Gold Canyon, AZ . We offer the latest in diagnostic and treatment technology to meet your needs.
Heel Spurs
Heel spurs are the result of calcium deposits that cause bony protrusions on the underside of the heel. Heel spurs are usually painless, but they have the potential to cause heel pain. Heel spurs tend to be associated with plantar fasciitis, which is a condition that causes inflammation of the band of connective tissue that runs along the bottom of the foot. They most often occur to athletes whose sports involve a lot of running and jumping.
Some risk factors for developing heel spurs include running and jogging on hard surfaces, being obese, wearing poorly fitting shoes, or having walking gait abnormalities.
It is possible to have a heel spur without showing signs of any symptoms. However, if inflammation develops at the point of the spur’s formation, you may have pain while walking or running. In terms of diagnosis, sometimes all a doctor needs to know is that the patient is experiencing a sharp pain localized to the heel to diagnose a heel spur. Other times, an x-ray may be needed to confirm the presence of a heel spur.
Heel spurs can be prevented by wearing well-fitting shoes that have shock-absorbent soles. You should also be sure that you are choosing the right shoe for the activity you want to partake in; for example, do not wear walking shoes when you want to go on a run. Additionally, maintaining a healthy weight can be beneficial toward preventing heel spurs, as it will prevent an excess amount of pressure being placed on the ligaments.
There are a variety of treatment options for people with heel spurs. Some of these include stretching exercises, physical therapy, shoe inserts, or taping and strapping to rest stressed muscles and tendons. If you have heel pain that lasts longer than a month, don’t hesitate to seek help from a podiatrist. Your doctor can help you determine which treatment option is best for you.
Arthritis Can Cause Pain in the Feet and Ankles
Why You Should Never Ignore Any Fracture in Your Toe
Fractures in the toes and metatarsals (long bones in the midfoot that connect to the toe bones) can be quite painful and should not be taken lightly. Breaks can either be traumatic (acute) that occur instantly due to an injury, or can be stress fractures which develop over time. Traumatic fractures can cause a bone to become misaligned in certain cases. You may hear a snap at the moment of impact and you may even notice that the toe is crooked or misshapen in some way. Pain may be felt at the site of the injury, and bruising and swelling may occur the following day. With a stress fracture, any pain felt while using the affected foot may subside when you rest, and although you may notice swelling there should be no apparent bruising. It is important to see a podiatrist for any broken bone in your toe or metatarsal, even if you have been treated initially at an emergency room. Proper treatment and rehabilitation will help avoid future complications like an improperly healed bone, mobility issues, difficulty wearing shoes, deformities, chronic pain, or arthritis in the joint.
A broken toe can be very painful and lead to complications if not properly fixed. If you have any concerns about your feet, contact John McGhan, DPM from Gold Canyon Foot & Ankle. Our doctor will treat your foot and ankle needs.
What to Know About a Broken Toe
Although most people try to avoid foot trauma such as banging, stubbing, or dropping heavy objects on their feet, the unfortunate fact is that it is a common occurrence. Given the fact that toes are positioned in front of the feet, they typically sustain the brunt of such trauma. When trauma occurs to a toe, the result can be a painful break (fracture).
Symptoms of a Broken Toe
- Throbbing pain
- Swelling
- Bruising on the skin and toenail
- The inability to move the toe
- Toe appears crooked or disfigured
- Tingling or numbness in the toe
Generally, it is best to stay off of the injured toe with the affected foot elevated.
Severe toe fractures may be treated with a splint, cast, and in some cases, minor surgery. Due to its position and the pressure it endures with daily activity, future complications can occur if the big toe is not properly treated.
If you have any questions please feel free to contact our office located in Gold Canyon, AZ . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
What to Know About a Broken Toe
Trauma to the foot, especially the toes, can occur in many ways. Banging them, stubbing them, or dropping something on them are a few different ways this trauma can occur. Given the fact that toes are positioned in front of the feet, they typically sustain the brunt of such trauma. When trauma occurs to a toe, the result can be a painful break or fracture. Another type of trauma that can break a toe is repeated activity that places stress on the toe for prolonged periods of time.
Broken toes can be categorized as either minor or severe fractures. Symptoms of minor toe fractures include throbbing pain, swelling, bruising on the skin and toenail, and the inability to move the toe with ease. Severe toe fractures require medical attention and are indicated when the broken toe appears crooked or disfigured, when there is tingling or numbness in the toe, or when there is an open, bleeding wound present on the toe.
Generally, a minor toe break will heal without long-term complications. However, it is important to discontinue activities that put pressure on the toe. It is best to stay off of the injured toe and immediately get a splint or cast to prevent any more additional movement of the toe bones. You can also immobilize your toe by placing a small cotton ball between the injured toe and the toe beside it. Then, tape the two toes together with medical tape. Swelling can be alleviated by placing an ice pack on the broken toe directly as well as elevating your feet above your head.
Severe toe fractures may be treated with a splint, cast, and in some cases, minor surgery, especially when the big toe has been broken. Due to its position and the pressure the big toe endures with daily activity, future complications can occur if it is not properly treated. Pain associated with minor toe fractures can be managed with over-the-counter pain medications. Prescription pain killers may be necessary for severe toe fractures.
The healing time for a broken toe is approximately four to six weeks. In severe cases where the toe becomes infected or requires surgery, healing time can take up to eight weeks or more. While complications associated with a broken toe are immediately apparent, it is important to note that there are rare cases when additional complications, such as osteoarthritis, can develop over time. You should immediately speak with your podiatrist if you think you have broken your toe due to trauma. They will be able to diagnose the injury and recommend the appropriate treatment options.
Vascular Testing in Podiatry
In foot care, vascular testing may be required in the diagnosing and treatment of certain podiatric conditions. Vascular testing is particularly relevant for patients with high-risk diabetes, poor circulation, peripheral artery disease (PAD), and chronic venous insufficiency (CVI). Procedures typically involve the examination of blood vessels throughout the body for blockages or buildup.
Vascular testing is very important for the diagnosis of various conditions, including peripheral artery disease and chronic venous insufficiency, as these conditions can greatly affect one’s quality of life and cause pain in the lower limbs. Circulatory problems in the feet and ankles can reflect issues throughout the body, making testing of the blood vessels pertinent.
Testing methods vary between practitioners and can be specific to certain foot and ankle problems. Modern technology has brought about the ability to perform vascular testing using non-invasive methods, such as the cuff-based PADnet testing device. This device records the Ankle-Brachial Index (ABI)/Toe-Brachial Index (TBI) values and Pulse Volume Recording (PVR) waveforms. Contact your podiatrist to determine what vascular testing is available for your needs.